Decoding Peri-Menopause
Peri-Menopause Decluttered, Including Links To Helpful Resources.
Perimenopause is a natural phase in a woman's life that marks the transition to menopause. This period can last several years and brings various physical, emotional, and hormonal changes. At Lightyears Health, we believe that knowledge is power, especially when it comes to understanding your body's changes.
Let's decode perimenopause, exploring what it is, how it affects your health, and how you can navigate this transition.
WHAT IS PERI-MENOPAUSE?
Perimenopause, derived from Greek, meaning "around menopause," is the phase leading up to menopause. It typically begins in a woman's 40s but can start as early as the mid-30s¹. During this time, your body gradually produces less oestrogen, leading to various symptoms and changes. This transition is a normal part of aging.
Key Facts
- Per a 2016 study, average age of menopause for Indian women is 46 years².
- The average duration of perimenopause is 4 years (this can range from 2-8 years).
- Menopause is documented when you go through 12 consecutive months without a menstrual period. This also marks the end of peri-menopause.
- Perimenopause is characterized by significant hormonal fluctuations, which have symptoms associated with them.
HORMONAL SYMPHONY DURING PERI-MENOPAUSE
Understanding the hormonal changes during perimenopause is crucial to comprehending the symptoms and bodily changes you may experience. The primary hormones involved in this transition are:
- Oestrogen: The main female sex hormone, responsible for regulating the menstrual cycle and supporting various bodily functions.
- Progesterone: Works in balance with oestrogen to regulate the menstrual cycle and prepare the uterus for pregnancy.
During perimenopause, these hormones undergo significant fluctuations:
- Oestrogen: Levels begin to fluctuate and gradually decline. However, this decline is not steady, and you may experience periods of oestrogen dominance followed by oestrogen deficiency³.
- Progesterone: Production decreases more steadily than oestrogen, often leading to cycles without ovulation (anovulatory cycles)⁴.
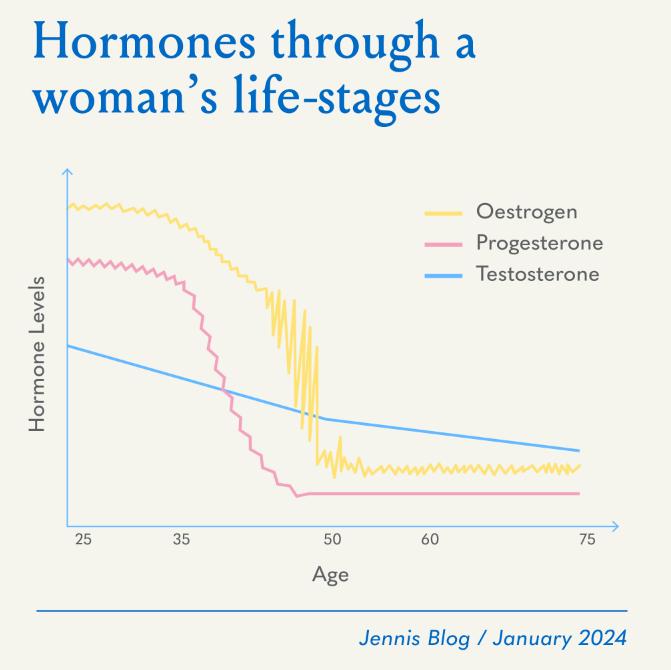
Note: This chart is a generalized representation. Individual experiences may vary.
COMMON SYMPTOMS OF PERI-MENOPAUSE
The hormonal fluctuations during perimenopause can lead to a variety of symptoms. It's important to note that every woman's experience is unique, and you may not experience all of these symptoms:
- Irregular periods: Your menstrual cycle may become longer, shorter, or skip months. This is often one of the first signs of perimenopause.
- Hot flashes and night sweats: Sudden feelings of heat, often accompanied by sweating and flushing. These are thought to be caused by the hypothalamus's response to declining oestrogen levels.
- Weight gain and slowed metabolism: Hormonal changes can affect how your body uses energy and stores fat, often leading to weight gain around the midsection⁵.
- Bone density loss: Accelerated loss of bone density due to declining oestrogen levels, increasing the risk of osteoporosis⁶.
- Joint pain: Oestrogen has anti-inflammatory properties, so its decline can lead to increased joint pain or stiffness⁷.
- Fatigue: Many women experience increased fatigue and lack of energy during perimenopause. This fatigue can be the result of a few different causes, including the hormonal changes expected with perimenopause and sleep disturbances.
- Mood changes: You may experience irritability, mood swings, or an increased risk of depression. These changes are linked to hormonal fluctuations and their effect on neurotransmitters.
- Sleep disturbances: Difficulty falling asleep or staying asleep, often related to night sweats or anxiety. Declining progesterone levels can affect sleep quality.
- Vaginal dryness: Decreased vaginal lubrication due to lower oestrogen levels, which can lead to discomfort during intercourse⁸.
- Changes in libido: You may experience a decrease or, sometimes, an increase in sex drive. This can be due to hormonal changes or a combination of physical and emotional factors⁹.
- Thinning hair and dry skin: Decreased oestrogen can affect hair and skin health, leading to increased dryness and potential hair thinning¹⁰.
MANAGING PERI-MENOPAUSE
While perimenopause is a natural process, there are numerous ways to manage its symptoms and support your overall health:
- Balanced nutrition: A diet rich in calcium, myo-inositol, vitamin D, and phytoestrogens can support bone health and help manage symptoms. Consider incorporating:
1. Calcium-rich foods: Dairy products, leafy greens, and fortified foods
2. Vitamin D sources: Fatty fish, egg yolks, and sunlight exposure - Regular exercise: Physical activity can help maintain a healthy weight, reduce stress, and improve sleep quality.
- Stress management: Chronic stress can exacerbate perimenopausal symptoms. Try techniques like:
1. Meditation or mindfulness practices
2. Deep breathing exercises
3. Progressive muscle relaxation
4. Regular leisure activities or hobbies - Hormone therapy: In some cases, your doctor may recommend hormone therapy to alleviate severe symptoms.
- Nutritional supplements: Supplements can help address specific perimenopausal concerns.
- Regular health check-ups. These include:
1. Annual physical exams
2. Periodic mammograms
3. Periodic pap smears
4. Bone density scans
5. Thyroid function tests
Remember, every woman's experience with perimenopause is unique. What works for one person may not work for another. It's essential to listen to your body, track your symptoms, and work closely with your healthcare provider to develop a personalized management plan.
Perimenopause is not just an ending but also a beginning – a transition into a new phase of life. With the right knowledge, support, and self-care, you can navigate this transition with confidence and embrace the changes it brings.
FURTHER READINGS
- Perimenopause, Mayo Clinic, 2023. LINK HERE
- Perimenopause, Johns Hopkins Medicine, 2021. LINK HERE
- Menopause 101: A Primer for the Perimenopausal & Early Menopause Symptoms, The North American Menopause Society, NAMS. LINK HERE
- Santoro, N. (2016) Perimenopause: From Research to practice, Journal of Women’s Health (2002). LINK HERE
- Perimenopause: Age, stages, signs, symptoms & treatment, Cleveland Clinic. LINK HERE
Citations
- Santoro, N. (2016). Perimenopause: From Research to Practice. Journal of Women's Health, 25(4), 332-339.
- Ahuja M. Age of menopause and determinants of menopause age: A PAN India survey by IMS. J Midlife Health. 2016 Jul-Sep;7(3):126-131. doi: 10.4103/0976-7800.191012. PMID: 27721640; PMCID: PMC5051232. [3] Harlow, S. D., et al. (2012). Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Fertility and Sterility, 97(4), 843-851.
- Burger, H. G., et al. (2007). A prospective longitudinal study of serum testosterone, dehydroepiandrosterone sulfate, and sex hormone-binding globulin levels through the menopause transition. The Journal of Clinical Endocrinology & Metabolism, 92(3), 1060-1067.
- Prior, J. C. (2005). Ovarian aging and the perimenopausal transition: the paradox of endogenous ovarian hyperstimulation. Endocrine, 26(3), 297-300.
- Davis, S. R., et al. (2012). Understanding weight gain at menopause. Climacteric, 15(5), 419-429.
- Finkelstein, J. S., et al. (2008). Bone mineral density changes during the menopause transition in a multiethnic cohort of women. The Journal of Clinical Endocrinology & Metabolism, 93(3), 861-868.
- Watt, F. E. (2018). Musculoskeletal pain and menopause. Post Reproductive Health, 24(1), 34-43.
- Nappi, R. E., & Lachowsky, M. (2009). Menopause and sexuality: prevalence of symptoms and impact on quality of life. Maturitas, 63(2), 138-141.
- Avis, N. E., et al. (2009). Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women's Health Across the Nation. Menopause, 16(3), 442-452.
- Birch, M. P., Messenger, J. F., & Messenger, A. G. (2001). Hair density, hair diameter and the prevalence of female pattern hair loss. British Journal of Dermatology, 144(2), 297-304.
